Double lung transplants weren’t typically recommended for lung cancer patients. But a new technique developed at Northwestern has been successful.
CHICAGO — For decades, double lung transplants were not considered a viable option for treating lung cancer.
“It had been done, but it had always failed,” said Ankit Bharat, chief of thoracic surgery at Northwestern Medicine. “When you took out the lungs, the cancer cells would spread to the rest of the body, and it would come back a matter of months after the transplant.”
But after developing a new technique to replace damaged lungs during the height of the COVID-19 pandemic, Northwestern Medicine’s Canning Thoracic Institute has now performed more than 40 successful lung transplants on cancer patients in just two and a half years.
The operation has a 100% success rate for lung cancer patients today, and in January the hospital completed its first transplant on a patient with lungs affected by both COVID-19 and lung cancer.
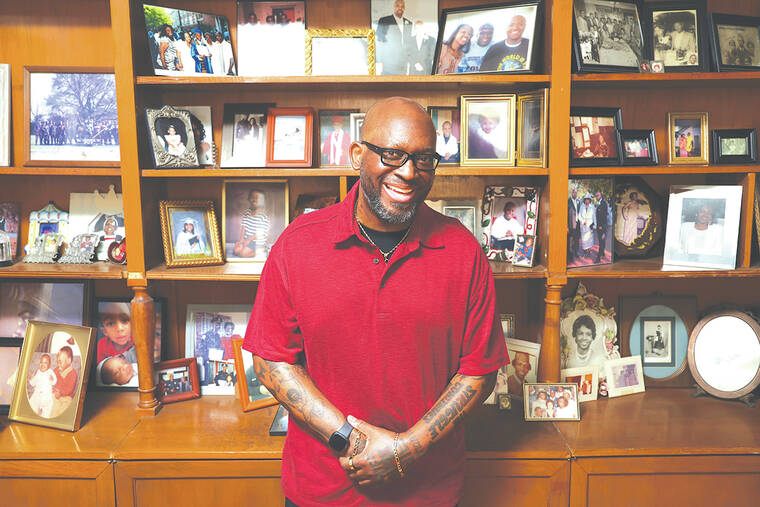
Art Gillespie, a captain with the University of Chicago Police Department, contracted COVID-19 in March 2020 while visiting his uncle in a nursing home. While hospitalized with the virus, Gillespie discovered he had Stage 1 lung cancer.
Though he received treatment for COVID and chemotherapy, he developed pulmonary fibrosis, a disease that causes scarring in the lungs and makes it difficult to breathe. Ultimately, Gillespie had two-thirds of his right lung removed to treat the cancer, and, despite the operation, needed daily oxygen.
Later, Gillespie received a one-to-two-year life expectancy prognosis.
“2022 was primarily me just becoming much more sick,” Gillespie said. “My quality of life at that point was pretty impacted. My ability to do anything, even speaking, was very taxing.”
Bharat said that Gillespie was a good candidate for a double lung transplant, especially because the transplant treatment for lung cancer had been directly developed from the technique for COVID-affected lungs.
While lung transplants had typically been performed by removing the lungs one by one, cutting first the vein that takes blood from the heart to the lungs and then the vein that takes it back, surgeons had to figure out a way that would prevent COVID bacteria from moving from the lungs to the heart, according to Bharat.
Doctors developed a technique to cut the veins simultaneously and later discovered the same technique could stop the spread of cancer cells.
Gillespie had the operation in January after being placed on the transplant list in September. He is on the way to a full recovery, he said, and hopes to return to work in the near future.
“I’m a grandfather,” Gillespie said. “The first thing I thought about was having that additional time to spend with (my grandkids), and watch them grow. That’s just an indescribable benefit.”